TOTAL KNEE REPLACEMENT SURGERY IN DELHI
Dr. Biren Nadkarni is a specialist Total Knee Replacement Surgeon in Delhi
Looking for Total Knee Replacement Surgery?
The knee joint is one of the most important joints of the body and it is responsible for carrying the major weight of the body. The knee joint is required to be healthy to carry on many essential routine activities. However, due to certain bone-related disorders such as degenerative disease (which is again of many types), the knee joint starts to degenerate and the person feels difficulty while walking or standing. Now depending upon the severity and grade, the treatments vary from Physiotherapy to medications to surgery in extreme cases. Sometimes walking supports are also used for making the patients walk properly.
This article provides comprehensive information about total knee replacement surgery, including its purpose, procedure, and potential benefits, making it a valuable resource for anyone considering this treatment option.
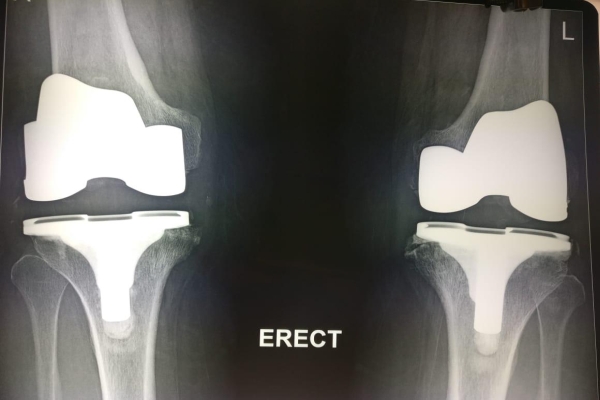
Before Surgery

After Surgery
Total Knee Replacement Anatomy
A new joint is made up of more than one bone just like any other joint of the body. What makes a knee joint special is that this joint has an extra cover over itself like the Patella (knee cap). This joint is a fusion of three bones- The Femur bone (thigh bone), the Tibia Bone (Shinbone), and the kneecap or patella bone. Besides the bones, the joint is also affixed using some ligaments. The joint is fixed from all the sides, anterior, posterior, medial, and lateral.
How does the Knee Joint start to malfunction?
It is not uncommon to witness people with shooting pain in the knee joint or facing difficulty in walking due to the pain in the knee joint. This pain can be caused due to various underlying reasons that we are going to discuss in our next sub-topic.
Etiology/Causes of Knee Pain
Below are some reasons behind chronic knee joint pain such as –
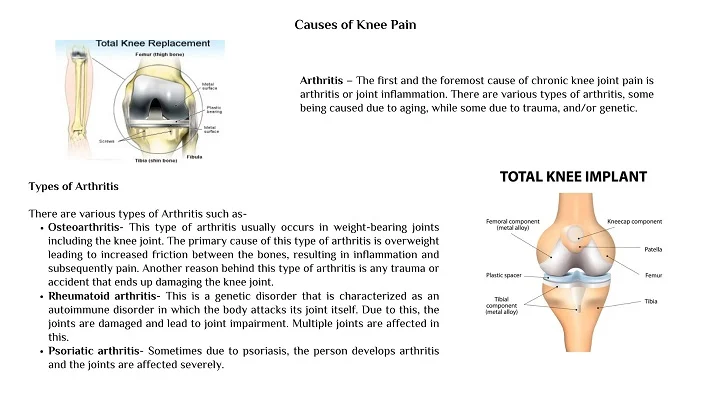
Trauma/Accident– Accidents or any other injuries are the second most reason for damaging the knee joints. The most common type of accident is a dashboard injury in which the knee joint gets hit and ligaments get torn up. The torn-up ligament results in the unstabilized knee joint and therefore, knee damage.
All the above reasons lead to knee joint damage and subsequent requirement for getting a knee joint replacement surgery (in severe cases).
What is Total Knee Replacement Surgery?
A Total Knee Joint Replacement or Knee Arthroplasty is a corrective joint surgery that is performed by an experienced Orthopaedic surgeon. For easy understanding, replacement surgery can also be called resurfacing surgery, as this surgery includes replacing the surfaces of the bones. Following are the basic steps involved:
- Preparation- The first step includes preparing the bones for an Arthroplastic procedure. This involves the removal of cartilage surfaces near the end of the bones along with the attached bony parts.
- Affixing the Metal parts- Next step includes replacing the removed cartilage and the bony parts with the metal parts. These metal parts are made in such a way that they fit perfectly over the bones’ surfaces, either fitted or cemented.
- Resurfacing of the Patellar Bone- In this step, the Patellar Bone is resurfaced in a way that it fixes the newly created joint surfaces. Some surgeons use a plastic button while resurfacing this bone.
- Spacer- At the last, a medically approved plastic spacer is inserted in between the metal components for smooth gliding movements
When Should One Get A Knee Replacement Surgery?
Deciding over the surgery is the sole decision of the person, his/her family, and the post-evaluation analyses of the joint by the Orthopedic surgeon.
Recommendations for a surgery–
Below are the chief examinations that may end up you getting surgery done-
- Severe level knee joint damage.
- Excessive stiffness even while doing basic work like walking, climbing the stairs, getting up, etc.
- The appearance of Fixed Formation Deformity (FFD) is bow-shaped legs.
- Pain while resting, both day and night.
- Failure of alternative treatments such as medications, physiotherapy, steroid injections, etc.
Total knee replacement Surgery Complications
There are certain complications that a patient might face after the surgical procedure-
- Formation of sepsis at the site of the incision. A small amount of infection is normal and treatable with normal antibiotics, but deep infection in any part of the body may prove harmful.
- Formation of blood clots (thrombosis). This is the most common post-surgical complication. It becomes worse when the clots (thrombus) break off from one point and travel to other parts of the body. This situation can be life-threatening. A condition called Deep Vein Thrombosis (DVT) is a dreaded life-threatening condition that requires serious medical attention.
- Surrounding tissues or nerve injuries may occur during the incision or surgical procedure.
Who is the Best Total Knee Replacement Surgeon in Delhi?
Dr. Biren Nadkarni is one of the best knee replacement surgeons in Delhi with an experience of more than 20 years in Orthopedic surgeries. He, with his team, has completed thousands of Orthopedic surgeries including joint replacement surgeries.
How a Patient is Prepared for Joint Replacement Surgery?
Dr. Biren Nadkarni is an extremely gentle human being besides being the best orthopedic surgeon. He examines his patients very carefully right from the moment the patient enters the hospital to his discharge and follow-up. He, with his team of highly proficient individuals, takes care of the patient greatly. The following steps are involved in examining the patient and preparing him for the surgery-
- Medical Care- Patient’s medical conditions are evaluated before operation much in advance, weeks before the operation. If the person has heart disease, he or she may be required to visit a cardiologist to get examined.
- Tests- Some biochemical tests may be prescribed to the patient to get a fair idea about the health status of the person and to make sure that there will not be any kind of complications post-surgery. These biochemical tests may be for your urine, blood, and other health statuses.
Dr. Biren Nadkarni expertise in evaluating his patients and only prescribes the surgery if the other forms of treatments fail. Besides taking care of the physical well-being of the person, he also takes care of his mental status. The patient is counseled like a family and is told about every little detail about the surgery, right from getting admitted to getting discharge and rehabilitation.
Total knee replacement Surgery
- The surgery is performed by Dr. Biren Nadkarni under the administration of anesthesia.
- The type of anesthesia depends upon the evaluation of the patient and is the decision of the anesthesiologist.
- Generally speaking, there are various types of anesthesia and in joint replacement surgery, the type of anesthesia involved are general anesthesia spinal, nerve block, or epidural anesthesia.
- The surgical procedure usually takes from one to two hours depending upon the conditions of the patient.
Total Knee Replacement Post-surgical Care
- Once the patient is operated on, he or she is not discharged immediately. The patient is kept under observation for any kind of medical problem.
- Observing pain after the surgery is natural and likely to develop. To relieve the patient from this pain, anti-analgesic drugs are prescribed to the patient which he has to take for a limited course of time.
- To eliminate the risk of blood clot formation, several measures are taken such as ankle-toe movements, blood thinners, supporting hose, etc.
- For regaining the lost range of movement and strength, a Physiotherapist-guided complete rehabilitation program is prescribed to the patient which can be taken while at the hospital stay and home after getting discharged. This is an essential step and the person should certainly consider getting physical therapy.
Home Care
Once the patient is discharged, proper care must be taken while at home like-
- Taking care of the wound properly and dressing it from time to time. You should also avoid drenching it until the wound is dried and healed.
- Exercising, which is an essential step. This should be done under the guidance of an experienced Physiotherapist only. He or she will make a complete program based on the conditions of the patient.
- It is also important to keep in mind that the patient should only start weight-bearing exercises after affirmation from the surgeon. Normal ROM exercises can be started right from the next day of the surgery to regain lost mobility.
FAQs
It usually takes around 6-8 weeks to completely recover from joint replacement surgery. This period may increase or decrease depending upon the individual’s condition.
